Connect With Us

Causes of Foot Stress Fractures

Metatarsal stress fractures, affecting the long bones in the foot, can vary in severity and type. Stress fractures, common in athletes and runners, result from repetitive impact or overuse, causing tiny cracks in the bone. These types of fractures typically develop gradually, causing pain, tenderness, and swelling that worsen with activity. Overuse, such as prolonged walking or running on hard surfaces without adequate rest, increases the risk of foot stress fractures. Proper diagnosis through imaging and treatment, including rest, immobilization, and sometimes surgery, is essential for recovery and preventing long-term complications associated with metatarsal fractures. If you have foot pain and believe you may have a stress fracture, it is suggested that you confer with a podiatrist who can properly diagnose and treat this type of foot injury.
Activities where too much pressure is put on the feet can cause stress fractures. To learn more, contact one of our podiatrists from Houston Foot and Ankle. Our doctors can provide the care you need to keep your pain free and on your feet.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures occur in the foot and ankle when muscles in these areas weaken from too much or too little use. The feet and ankles then lose support when walking or running from the impact of the ground. Since there is no protection, the bones receive the full impact of each step. Stress on the feet can cause cracks to form in the bones, thus creating stress fractures.
What Are Stress Fractures?
Stress fractures occur frequently in individuals whose daily activities cause great impact on the feet and ankles. Stress factors are most common among:
- Runners
- People affected with Osteoporosis
- Tennis or basketball players
- Gymnasts
- High impact workouts
Symptoms
Pain from the fractures occur in the area of the fractures and can be constant or intermittent. It will often cause sharp or dull pain with swelling and tenderness. Engaging in any kind of activity which involves high impact will aggravate pain.
If you have any questions please feel free to contact our offices located in Kingwood, Humble, The Woodlands, and Conroe, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Stress Fractures of the Foot and Ankle
Our bones are important aspects of our body and they are constantly changing. The heavier the workload for a bone, the more likely it is that calcium will be placed in it. When a bone isn’t used often, there won’t be much calcium within it. When stress from repetitive loads prevent the bone from being able to repair itself, cracks will start to form. Stress fractures are defined as cracks in a bone that result from repetitive force, such as overuse.
The most common cause of stress fractures is a sudden increase in intensity and duration of physical activity. For example, if you begin to run long distances without working your way into doing so, you will be more likely to develop a stress fracture.
Common symptoms of stress fractures are pain and swelling near the weight bearing area on the injured bone. When initial x-rays are performed, it is possible that the fracture will not show up. However, once the stress on the area continues, the damage will increase, and the fracture will be severe enough to show up on an x-ray. Certain parts of the foot are more likely to develop stress fractures than others. Areas that typically have these fractures are: the metatarsals, the navicular bone, the calcaneus, tibia, and fibula.
Since women are at an increased risk of developing osteoporosis, they are twice as likely as men to sustain a stress fracture. Additionally, old age causes a decrease in bone mineral density which is why elderly people are also likely to develop these fractures.
It is important for you to be professionally diagnosed by a podiatrist if you suspect you have a stress fracture, because there are other injuries that can easily be mistaken for a fracture. Sprains, strains, shin splints, plantar fasciitis, and Morton’s neuroma can all easily be mistaken for stress fractures in the foot. Your podiatrist will likely ask you a series of questions to determine what type of pain you are experiencing. These questions will help your doctor identify whether you have a stress fracture.
The best method of treatment for a stress fracture is rest. Additionally, a walking boot, cast, or crutches, will help rest the area that is injured. The typical healing time for stress fractures is 4-12 weeks, however this depends on which bone is involved.
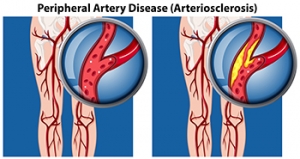
How Peripheral Artery Disease Affects the Feet
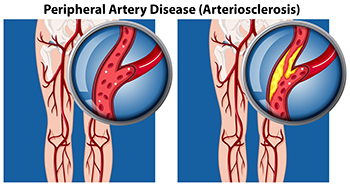
Peripheral artery disease, or PAD, affects blood circulation, often manifesting through symptoms related to the feet. Common signs include cramping, pain, or numbness in the feet during physical activity, which subsides with rest. Coldness or discoloration of the feet or toes, particularly in comparison to the unaffected leg, may also occur due to reduced blood flow. Slow-healing wounds or sores on the feet are another indicator, as PAD limits the delivery of oxygen and nutrients essential for tissue repair. PAD, caused by narrowed arteries due to plaque buildup, increases the risk of complications, such as infections and tissue death in severe cases. Regular foot exams from a podiatrist are essential for managing PAD. If you have symptoms of PAD, it is suggested that you are under the care of this type of doctor who can help you to manage this condition.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with one of our podiatrists from Houston Foot and Ankle. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our offices located in Kingwood, Humble, The Woodlands, and Conroe, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Types of Hammertoe Surgery and Potential Risks

Hammertoe surgery aims to correct deformities where a toe bends abnormally at the middle joint. Types of surgery include tendon transfer, where a tendon is rerouted to pull the toe into the correct position, and joint resection, which involves removing part of the joint to straighten the toe. Fusion surgery permanently joins the bones in the affected joint, ensuring the toe remains straight. While these procedures can effectively alleviate pain and improve function, they carry potential risks. Complications may include infection, nerve damage, and prolonged swelling. Additionally, there is a possibility of stiffness or recurrence of the deformity. Consulting with a podiatrist ensures a thorough understanding of the benefits and risks. If you are considering surgery for this condition, it is suggested that you consult with this type of doctor who can determine if this is a right decision for you.
Foot surgery is sometimes necessary to treat a foot ailment. To learn more, contact one of our podiatrists of Houston Foot and Ankle. Our doctors will assist you with all of your foot and ankle needs.
When Is Surgery Necessary?
Foot and ankle surgery is generally reserved for cases in which less invasive, conservative procedures have failed to alleviate the problem. Some of the cases in which surgery may be necessary include:
- Removing foot deformities like bunions and bone spurs
- Severe arthritis that has caused bone issues
- Cosmetic reconstruction
What Types of Surgery Are There?
The type of surgery you receive will depend on the nature of the problem you have. Some of the possible surgeries include:
- Bunionectomy for painful bunions
- Surgical fusion for realignment of bones
- Neuropathy decompression surgery to treat nerve damage
Benefits of Surgery
Although surgery is usually a last resort, it can provide more complete pain relief compared to non-surgical methods and may allow you to finally resume full activity.
Surgical techniques have also become increasingly sophisticated. Techniques like endoscopic surgery allow for smaller incisions and faster recovery times.
If you have any questions please feel free to contact our offices located in Kingwood, Humble, The Woodlands, and Conroe, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Foot and Ankle Surgery
When conservative, noninvasive methods prove ineffective, surgery may be selected as the next course of action for the treatment of your foot or ankle condition. A wide number of foot and ankle surgical procedures exist, and it is up to your podiatrist to determine which intervention will be most appropriate and helpful for your case. Some surgical procedures include bunion surgery, fusion, hammertoe surgery, heel spur surgery, metatarsal surgery, nail surgery, neuroma surgery, reconstructive surgery, skin surgery, and tendon surgery. Typically, surgery is turned to as a definitive way to alleviate excessive pain or discomfort and to return your foot to full mobility.
Regardless of the location on the body, all surgical procedures require preoperative testing and examination to ensure the surgery’s success and preferred outcome. A review of your medical history and medical conditions will take place, as will an evaluation of any current diseases, illnesses, allergies, and medications. Tests such as blood studies, urinalyses, EKG, X-rays, and blood flow studies may be ordered. Because the procedure involves the foot and/or ankle, the structures of your feet while walking may also be observed by your podiatrist.
Care post-surgery will depend on the type of surgical procedure performed. Typically, all postoperative care involves rest, ice, compression, and elevation. To improve and ensure a safe recovery, your foot and ankle surgeon may also employ the use of bandages, splints, surgical shoes, casts, crutches, or canes. He will also determine if and when you can bear weight. A timely and thorough recovery is a priority for both you and your podiatrist, and carefully following postoperative instructions can help achieve this.
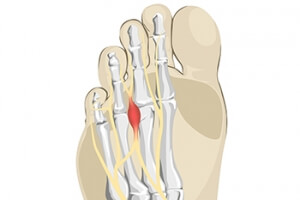
Definition and Symptoms of Morton’s Neuroma
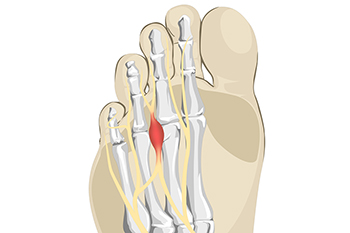
Morton's neuroma is a painful condition affecting the ball of the foot, commonly between the third and fourth toes. It occurs when the tissue surrounding one of the nerves leading to the toes thickens, causing sharp, burning pain in the ball of the foot. Symptoms often include a sensation of standing on a pebble, tingling, or numbness in the toes. The pain may worsen with activities like walking or wearing tight shoes. Patients often describe a feeling of something being caught in the shoe or a persistent discomfort in the forefoot. Identifying and addressing these symptoms early can help manage the condition and prevent further complications. If you are experiencing any of the above sensations, it is suggested that you confer with a podiatrist who can diagnose and treat Morton’s neuroma.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact one of our podiatrists of Houston Foot and Ankle. Our doctors will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our offices located in Kingwood, Humble, The Woodlands, and Conroe, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Morton's Neuroma
A neuroma is a thickening of nerve tissue and can develop throughout the body. In the foot, the most common neuroma is a Morton’s neuroma; this typically forms between the third and fourth toes. The thickening of the nerve is typically caused by compression and irritation of the nerve; this thickening can in turn cause enlargement and, in some cases, nerve damage.
Neuromas can be caused by anything that causes compression or irritation of the nerve. A common cause is wearing shoes with tapered toe boxes or high heels that force the toes into the toe boxes. Physical activities that involve repeated pressure to the foot, such as running or basketball, can also create neuromas. Those with foot deformities, such as bunions, hammertoes, or flatfeet, are more likely to develop the condition.
Symptoms of Morton’s neuroma include tingling, burning, numbness, pain, and the feeling that either something is inside the ball of the foot or that something in one’s shoe or sock is bunched up. Symptoms typically begin gradually and can even go away temporarily by removing one’s shoes or massaging the foot. An increase in the intensity of symptoms correlates with the increasing growth of the neuroma.
Treatment for Morton’s neuroma can vary between patients and the severity of the condition. For mild to moderate cases, padding, icing, orthotics, activity modifications, shoe modifications, medications, and injection therapy may be suggested or prescribed. Patients who have not responded successfully to less invasive treatments may require surgery to properly treat their condition. The severity of your condition will determine the procedure performed and the length of recovery afterwards.
Common Symptoms of Gout

Gout is a form of arthritis characterized by sudden, intense pain, often in the big toe, but it can affect other joints as well. The pain is typically described as sharp, throbbing, or excruciating, making even the lightest touch unbearable. In addition to the pain, affected joints often become swollen, red, and warm to the touch. These symptoms can come on suddenly, often at night, and can last for several days or even weeks. During a gout attack, movement of the affected joint is extremely painful, and the skin around the joint can appear shiny and stretched. Some individuals might also experience a lingering discomfort even after the severe pain subsides, along with decreased mobility in the joint. Chronic gout can lead to persistent pain and can cause damage to the joints over time. If you have pain in your big toe, it is strongly suggested that you consult a podiatrist.
Gout is a foot condition that requires certain treatment and care. If you are seeking treatment, contact one of our podiatrists from Houston Foot and Ankle. Our doctors will treat your foot and ankle needs.
What Is Gout?
Gout is a type of arthritis caused by a buildup of uric acid in the bloodstream. It often develops in the foot, especially the big toe area, although it can manifest in other parts of the body as well. Gout can make walking and standing very painful and is especially common in diabetics and the obese.
People typically get gout because of a poor diet. Genetic predisposition is also a factor. The children of parents who have had gout frequently have a chance of developing it themselves.
Gout can easily be identified by redness and inflammation of the big toe and the surrounding areas of the foot. Other symptoms include extreme fatigue, joint pain, and running high fevers. Sometimes corticosteroid drugs can be prescribed to treat gout, but the best way to combat this disease is to get more exercise and eat a better diet.
If you have any questions please feel free to contact our offices located in Kingwood, Humble, The Woodlands, and Conroe, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.