Connect With Us
Blog

Options for Ingrown Toenail Surgery

Ingrown toenails develop when the edge of the nail grows into the surrounding skin, leading to pain, redness, swelling, and sometimes infection. Causes include improper nail trimming, tight shoes, toe injuries, or naturally curved nails. The area may feel sore, swollen, and, in more severe cases, may produce drainage or pus. When conservative treatments like warm soaks, antibiotics, or lifting the nail fail, a podiatrist may recommend a minor surgical procedure. One common option is partial nail avulsion, where only the ingrown portion is removed. Another method is a wedge resection, where the side of the nail and a portion of the nail bed are removed to stop the problematic section from growing back. These in-office procedures are quick, performed under local anesthesia, and typically offer long-term relief. If you have a painful ingrown toenail, it is suggested that you schedule an appointment with a podiatrist who can determine if surgery is right for you.
Foot surgery is sometimes necessary to treat a foot ailment. To learn more, contact one of our podiatrists of Houston Foot and Ankle. Our doctors will assist you with all of your foot and ankle needs.
When Is Surgery Necessary?
Foot and ankle surgery is generally reserved for cases in which less invasive, conservative procedures have failed to alleviate the problem. Some of the cases in which surgery may be necessary include:
- Removing foot deformities like bunions and bone spurs
- Severe arthritis that has caused bone issues
- Cosmetic reconstruction
What Types of Surgery Are There?
The type of surgery you receive will depend on the nature of the problem you have. Some of the possible surgeries include:
- Bunionectomy for painful bunions
- Surgical fusion for realignment of bones
- Neuropathy decompression surgery to treat nerve damage
Benefits of Surgery
Although surgery is usually a last resort, it can provide more complete pain relief compared to non-surgical methods and may allow you to finally resume full activity.
Surgical techniques have also become increasingly sophisticated. Techniques like endoscopic surgery allow for smaller incisions and faster recovery times.
If you have any questions please feel free to contact our offices located in Kingwood, Humble, The Woodlands, and Conroe, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Foot Surgery
In most cases, foot surgery is often chosen as the last available option for conditions that have otherwise been unsuccessfully treated. Surgery may be necessary for several reasons, including the removal of foot deformities (e.g. bone spurs or bunions), arthritis problems, reconstruction due to injury, and congenital malformations (e.g. club foot or flat feet). Regardless of one’s age, foot surgery may be the only successful option for treatment for certain conditions.
The type of surgery one undergoes depends on the type of foot condition the patient has. For the removal of a bunion growth, a bunionectomy is necessary. If the bones in the feet need to be realigned or fused together, a surgical fusion of the foot is needed. For pain or nerve issues, a patient may require surgery in which the tissues surrounding the painful nerve are removed. Initially, less invasive treatments are generally attempted; surgery is often the last measure taken if other treatments are unsuccessful.
While in many cases surgery is often deemed as the final resort, choosing surgery comes with certain benefits. The associated pain experienced in relation to the particular condition is often relieved with surgery, allowing patients to quickly resume daily activities. The greatest benefit, however, is that surgery generally eliminates the problem immediately.
Podiatry history has shown that foot treatments continue to evolve over time. In the field of foot surgery, endoscopic surgery is just one of the many advanced forms of surgery. As technology vastly improves so too will the various techniques in foot surgery, which already require smaller and smaller incisions with the use of better and more efficient tools. Thanks to such innovations, surgery is no longer as invasive as it was in the past, allowing for faster and easier recoveries.
Plantar Warts Can Cause Discomfort

Plantar warts are small, rough growths that appear on the bottom of the foot, usually on weight-bearing areas like the heel or ball of the foot. They are caused by the human papillomavirus, or HPV, which enters the skin through tiny cuts or cracks, often in places like public showers, gyms, or pool areas. Plantar warts may look like a callus, but often have a rough surface with black dots, which are tiny clotted blood vessels, at the center. The warts can be painful, especially while walking or standing, as pressure pushes them deeper into the skin. A podiatrist can diagnose plantar warts and offer effective treatments that go beyond over-the-counter options. These may include cryotherapy, topical acids, immune-boosting treatments, or minor surgical removal. Custom orthotics may also be recommended to reduce pressure on the area during healing. If you have a painful plantar wart, it is suggested that you schedule an appointment with a podiatrist for appropriate treatment.
Plantar warts can be very uncomfortable. If you need your feet checked, contact one of our podiatrists from Houston Foot and Ankle. Our doctors will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our offices located in Kingwood, Humble, The Woodlands, and Conroe, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Warts
Plantar warts are growths that typically appear on the heels or other weight-bearing areas of the feet. These warts are caused by the human papillomavirus (HPV). The virus enters the body through breaks in the skin, such as cuts, that are on the bottom of the feet. Plantar warts are more likely to affect children and teenagers, people with weakened immune systems, people who have a history with plantar warts, and people who walk barefoot in environments exposed to a wart-causing virus.
If you suspect you have plantar warts, you may have the following symptoms: pain or tenderness while walking, a lesion that interrupts the ridges in the skin of your foot, small fleshy lesions on the bottom of the foot, or a callus where a wart has grown inward over a well-defined spot on the skin.
HPV causes plantar warts to form and is very common. There are more than 100 kinds of the virus in existence. However, only a few of them cause warts on the feet. The other types of HPV are likely to cause warts on other parts of the body.
If you have plantar warts, your podiatrist may try different treatment methods depending on your specific case. Some treatments for plantar warts are peeling medicines (salicylic acid), freezing medicines (cryotherapy), or surgical procedures. Laser treatments and vaccines are also used to treat plantar warts.
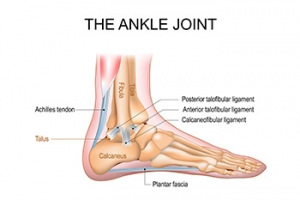
Foot and Ankle Structure and Function
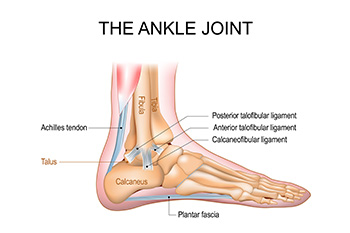
The foot and ankle form a complex structure designed for stability, mobility, and weight-bearing. The talocrural joint, commonly known as the ankle joint, connects the tibia, fibula, and talus. It allows for up and down movement of the foot, essential for walking and running. Beneath it lies the subtalar joint, which connects the talus and calcaneus bones and enables side-to-side motion, helping the foot adapt to uneven surfaces. The midtarsal joint, also called the transverse tarsal joint, includes the talonavicular and calcaneocuboid joints. This joint helps with rotational movement and flexibility. Together, these joints allow the foot and ankle to support body weight, absorb shock, and provide the motion needed for movement, balance, and overall function during daily activities. If you have injured your foot or ankle, it is suggested that you consult a podiatrist who can treat various foot conditions.
If you have any concerns about your feet, contact one of our podiatrists from Houston Foot and Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
Biomechanics in Podiatry
Podiatric biomechanics is a particular sector of specialty podiatry with licensed practitioners who are trained to diagnose and treat conditions affecting the foot, ankle and lower leg. Biomechanics deals with the forces that act against the body, causing an interference with the biological structures. It focuses on the movement of the ankle, the foot and the forces that interact with them.
A History of Biomechanics
- Biomechanics dates back to the BC era in Egypt where evidence of professional foot care has been recorded.
- In 1974, biomechanics gained a higher profile from the studies of Merton Root, who claimed that by changing or controlling the forces between the ankle and the foot, corrections or conditions could be implemented to gain strength and coordination in the area.
Modern technological improvements are based on past theories and therapeutic processes that provide a better understanding of podiatric concepts for biomechanics. Computers can provide accurate information about the forces and patterns of the feet and lower legs.
Understanding biomechanics of the feet can help improve and eliminate pain, stopping further stress to the foot.
If you have any questions please feel free to contact our offices located in Kingwood, Humble, The Woodlands, and Conroe, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Biomechanics in Podiatry
Podiatry is a branch of medicine that deals with the study, diagnosis, and treatment of foot and ankle conditions. There are various subdivisions in podiatry; biomechanics is one of them. Biomechanics is the way in which the bones, muscles, and joints of the feet and lower limb interact with each other.
Our feet play crucial roles in the way we move, and it is rare to have feet that are completely symmetrical. Common biomechanical issues include high or low arches or uneven leg heights. Excessive pronation often leads to fallen arches, or flat feet, and is a common cause of running injuries. People whose feet are over-pronated tend to have flexible and unstable feet. Pain is usually experienced during walking and running.
At times, people may be able to adapt to these abnormalities without any difficulties, but in other cases, these issues can cause a great deal of pain. This pain occurs because the joints, muscles, ligaments, and tendons are put under an excess amount of stress during movement. Common symptoms of biomechanical problems stemming from the feet include hip pain, knee pain, leg cramps, ankle pain, lower back pain, weak ankles, tripping, heel pain, Achilles pain, and shin splints.
Many biomechanical issues can be treated with orthotics. Orthotics are shoe insoles that are used to help control the way the foot operates. They can provide relief from foot pain, heel pain, and knee pain. Depending on your specific case, you may need to purchase over-the-counter orthotics or custom orthotics to fit your feet. Your podiatrist will be able to prescribe the perfect orthotic for your feet to help you walk around with ease.
Gait is defined as the way we move our bodies from one point to another. This is usually done by either walking or running. Gait analysis is a method used to assess the way we walk or run to highlight biomechanical abnormalities. Gait analyses are a great way to take a detailed look at how you walk and how your foot moves while you walk. An examination of the feet will help your podiatrist understand why you are suffering pain in other parts of your body.
Common Foot Problems Caused by Diabetes

Diabetes can lead to a range of serious foot problems due to its impact on circulation and nerve function. One of the most common complications is neuropathy, which causes tingling, numbness, or pain and reduces the ability to feel injuries. Peripheral artery disease can further restrict blood flow, slowing healing, and increasing the risk of infection. Foot ulcers may develop from unnoticed cuts or pressure points and can become severe without prompt care. Diabetic blisters, although painless, can appear suddenly and may become infected if not treated properly. Additionally, edema, or swelling in the feet and ankles, is another frequent issue and may indicate worsening circulation. If you have diabetes, it is strongly suggested that you consult a podiatrist who can provide proper foot care and regular checkups, which are essential for managing diabetes and preventing long-term complications.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact one of our podiatrists from Houston Foot and Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our offices located in Kingwood, Humble, The Woodlands, and Conroe, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetic Foot Conditions
Diabetes is the condition in which the body does not properly process food for use as energy. People with Type 1 diabetes cannot produce insulin, which is required for glucose to feed your body’s cells. It is typically caused by the immune system mistaking healthy cells for foreign invaders and destroying the insulin-producing cells in the pancreas. On the other hand, people with Type 2 diabetes cannot respond to insulin properly, and eventually cannot produce enough. The Centers for Disease Control and Prevention reports that over 30 million people in the United States have diabetes, with 1 in 4 having no idea they have it. Surprisingly, diabetes is the seventh leading cause of death in the US. The symptoms of diabetes include frequent urination, fatigue, hunger, and even blurry vision.
Diabetes can also affect the feet as well. Over time, diabetes can cause nerve damage to your feet, which could then lead to symptoms such as tingling, pain and numbness in the feet. Neuropathy can be very dangerous to a person with diabetes, since it prevents them from feeling injuries such as cuts or blisters in the feet, and if not detected early enough, may lead to infection. Neuropathy can also lead changes in the shape of your feet and toes. The best way for people with diabetes to prevent or delay neuropathy is keeping their blood glucose levels in their target range. This consists of eating right, having the correct amount of exercise, and taking medications.
Diabetes can also create calluses and foot ulcers as well. Calluses build up faster and occur more frequently with those affected by diabetes. If there are too many calluses, therapeutic shoes and inserts may be required. It is important to have calluses trimmed by a health professional, as doing it yourself may lead to infections. If these calluses continue to develop and thicken, they can lead to foot ulcers. Foot ulcers are open sores, that appear on the ball of the foot or on the bottom of the big toe. These ulcers can lead to future infections if not treated and may possibly result in losing a limb. It is important to report any ulcers to your podiatrist right away. Your doctor may take x-rays to examine the foot and clean out any dead and infected tissue.
Lastly, diabetes can also lead to poor circulation and peripheral arterial disease (PAD). The poor circulation in the feet and leg area is a result of diabetes narrowing and hardening, eventually slowing down the blood flow in that area. The best way to prevent this is to keep away from smoking and follow your doctor’s advice for maintaining blood pressure and cholesterol. PAD is similar to this complication. PAD is when blood vessels narrow or are blocked by fatty deposits. PAD also increases your risk of heart attacks and strokes and is a common condition to those affected by diabetes. The combination of both PAD and neuropathy may lead to infections and can result in amputation of certain limbs. PAD can be prevented with wearing the proper foot wear and regularly taking care of your feet.
If you want to take care of your feet, you should wash and dry them carefully and perform daily inspections to check for cuts, blisters, or swelling. Any physical activity you partake in should be approved by your health care provider. You should also be sure to wear special shoes if advised to do so by your doctor.
Types of Toe Deformities

Toe deformities are structural issues that may develop from birth or result from other factors. Common causes of toe deformities include wearing improper footwear, trauma, or joint and nerve conditions. Among the deformities are hammertoe, which involves a bend at the middle joint, and mallet toe, which affects the joint near the nail. Claw toe, where the toe curls under the foot, and overlapping toe, where one toe rests on another are other toe deformities. Curly toe is a congenital toe deformity in which one or more toes, usually the third or fourth, curl under due to tight tendons pulling them downward. Causes may include heredity, poorly fitting shoes, foot injuries, nerve damage from conditions like diabetes, or joint disorders like rheumatoid arthritis. These toe deformities can cause pain, limit mobility, and lead to complications like corns, open sores, and joint stiffness. When a toe deformity becomes rigid or painful, a podiatrist can offer medical treatment. Options include custom orthotics to reduce pressure and improve alignment or splints to support toe positioning. In severe cases, surgery may be required to straighten the toe and relieve discomfort. If you have a problematic toe deformity, it is suggested that you schedule an appointment with a podiatrist for appropriate treatment.
Toe pain can disrupt your daily activities. If you have any concerns, contact one of our podiatrists of Houston Foot and Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Causes Toe Pain?
Most severe toe pain is caused due to a sports injury, trauma from dropping something heavy on the toe, or bumping into something rigid. Other problems can develop over time for various reasons.
Toe pain can be caused by one or more ailments. The most common include:
- Trauma
- Sports injury
- Wearing shoes that are too tight
- Arthritis
- Gout
- Corns and calluses
- Hammertoe
- Bunions
- Blisters
- Ingrown toenails
- Sprains
- Fractures (broken bones)
- Dislocations
When to See a Podiatrist
- Severe pain
- Persistent pain that lasts more than a week
- Signs of infection
- Continued swelling
- Pain that prevents walking
Diagnosis
In many cases the cause of toe pain is obvious, but in others, a podiatrist may want to use more advanced methods to determine the problem. These can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatments for toe pain and injuries vary and may include shoe inserts, padding, taping, medicines, injections, and in some cases, surgery. If you believe that you have broken a toe, please see a podiatrist as soon as possible.
If you have any questions please feel free to contact our offices located in Kingwood, Humble, The Woodlands, and Conroe, TX . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.